News Release
July 17, 2019
CMS Announces 2019 Medicare ACO Class
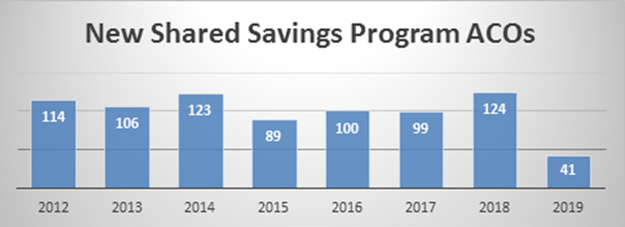
Slowed Growth Follows Numerous Program Changes
WASHINGTON —The National Association of Accountable Care Organizations (NAACOS) today congratulated new ACOs that joined the Medicare Shared Savings Program (MSSP) effective July 1. Roughly 40 new ACOs entered the program, which is less than the more than 100 new ACOs the program averaged in its first seven years. With the 2019 class, the MSSP grew by 400,000 beneficiaries, while prior years have seen growth of more than a million beneficiaries each year.
The next opportunity to join will be in January 2020 when the program returns to its typical schedule of ACOs joining at the start of the calendar year. The MSSP is the largest value-based payment program operated by the Centers for Medicare & Medicaid Services (CMS), and program results have steadily improved in recent years.
“This is a pivotal time for the transition to value, and we need to accelerate ACO adoption to effectively bend the Medicare cost curve,” said Clif Gaus, Sc.D., NAACOS president and CEO. “We hope this smaller class is only a reflection of an off-cycle start date and not an indication that the program and transition to value are slowing down.”
CMS made significant changes to the ACO program last year, a number of which were met with concern by the ACO industry, such as reduced shared savings opportunities and a faster pace to risk. The new “Pathways to Success” program structure is in place as of this month, though existing ACOs had the option to complete their current agreement periods under the previous rules before shifting to the new program structure. Overall, 518 ACOs are now in the MSSP, compared to 561 last year.
Returning ACOs should be congratulated for their commitment to value-based care,” Gaus said. “But NAACOS’ concern last year dealt largely with the pipeline of new ACOs, which today’s participation numbers call into question. This slowing growth will shrink the pool of future, risk-taking ACOs, which CMS should concern itself with.”
Accountable care, coordinated care, paying for the value of services delivered and not the volume, is the direction we should be moving our health system,” Gaus said. “ACOs are working to make that a reality, and NAACOS will continue to advocate for program changes to support their efforts.”
Data increasingly show ACOs are reducing Medicare spending. Earlier this month, the Medicare Payment Advisory Commission reported MSSP reduced spending between 1 and 2 percent from 2013 to 2016, which translates into tens of billions of dollars when compounded annually. An independent analysis commissioned by NAACOS and conducted last year by a health economics and policy consulting firm showed $2.7 billion in overall savings and more than $660 million in net savings, after paying shared savings to ACOs. Data from 2017, the most recent available, show ACO saved $1.1 billion compared to their CMS-set spending targets, a crude measure that undervalues ACO savings.
