September 11, 2023
The Honorable Chiquita Brooks-LaSure
Administrator
Centers for Medicare and Medicaid Services
U.S. Department of Health and Human Services
Attention: CMS-1784-P
Submitted electronically to regulations.gov
RE: CY2024 Medicare Physician Fee Schedule Proposed Rule
Dear Administrator Brooks-LaSure:
The National Association of ACOs (NAACOS) appreciates the opportunity to submit comments in response to CY2024 Medicare Physician Fee Schedule (MPFS) and Medicare Shared Savings Program (MSSP) proposed rule. NAACOS represents more than 400 accountable care organizations (ACOs) in Medicare, Medicaid, and commercial insurance working on behalf of health systems and physician provider organizations across the nation to improve quality of care for patients and reduce health care cost. NAACOS members serve over 8 million beneficiaries in Medicare value-based payment models, including the MSSP and the ACO Realizing Equity, Access, and Community Health (REACH) Model, among other alternative payment models (APMs).
NAACOS is pleased that CMS continues to work improve and enhance MSSP. Many of the proposed MSSP policies are responsive to concerns and suggestions raised by our members. Additionally, several physician payment policies better support team-based care and recognize the effort needed to address patients with complex needs; these services are building blocks toward population health. We thank CMS for their attention to these issues and ask that CMS employ policies that will encourage more rapid adoption of ACOs and population health.
NAACOS supports CMS’s stated goal of having all Medicare beneficiaries in a relationship accountable for quality and total cost of care by 2030. As the only permanent total cost of care model, CMS must ensure that current MSSP participants remain in the model and that the model attracts new clinicians and other providers. CMS should do the following to accomplish this goal:
- Address the benchmark ratchet. Over the next two years, the majority of MSSP participants will enter new contract agreements and have their benchmarks rebased and lowered due to achieving savings during the current contract cycle. While CMS has adopted policies to reduce the impact of the ratchet (i.e., prior savings adjustment, ACPT) these policies do not go far enough and many ACOs may face deep reductions to their benchmarks. It is critical that we ensure that ACOs have fair and accurate benchmarks. The savings achieved in these models directly impact patient care by expanding care teams, providing additional beneficiary services that are not billed to Medicare, ensuring provider retention with enhanced provider payment, and investing in technology or other services that enable care coordination and population health management. Lowering benchmarks because of the ratchet effect reduces providers’ ability to improve care and reduces the ACO’s opportunity to achieve success and reinvest shared savings into beneficiary care.
- Remove burden from the program. Beyond payment incentives, reduction of the fee-for-service (FFS) burden is a key recruitment tool to bring clinicians into the ACO model. We are concerned that certain policies (e.g., eCQM reporting, PI reporting for QPs, beneficiary notification) are increasing burden within the program. Entering a population health program requires significant effort to redesign care processes. Clinicians in an ACO model should be rewarded with burden reduction. CMS should examine all policies and ensure that the ACO program is not introducing new regulatory burdens.
- Support inclusion of all providers within the model. ACOs are a unique opportunity to coordinate care across the continuum. While providers across the continuum participate in ACOs, more can be done to bring additional providers into the model. We encourage CMS to offer primary care population based payments to increase primary care participation, encourage specialist engagement in ACOs, and provide additional technical support for provider participants that are not paid under the PFS (e.g., FQHC, RHC, CAH).
- Strengthen nonfinancial incentives within the model. Despite the Innovation Center’s testing of several waivers in ACO demonstrations, waivers available to MSSP ACOs have been limited. CMS must rapidly expand MSSP waivers and should create a process to accept public nominations for waivers in MSSP, similar to the process by which the public could annually request additions to the Medicare telehealth services list. Creating a transparent process for adding new waivers to MSSP would increase ACOs’ flexibility to meet the needs of their populations and support CMS’s goal to advance accountable care.
PHYSICIAN PAYMENT
Physician Payment
CMS proposes a CY 2024 Medicare conversion factor (CF) of $32.75, a decrease of 3.34 percent from the 2023 CF rate of $33.89. NAACOS is concerned that continual cuts create a disincentive for clinicians to adopt population health models. When physician payment is cut it is difficult to encourage clinicians to adopt a model that could potentially further reduce compensation through discounts or savings targets. We must ensure that clinicians in FFS receive adequate payment and build additional financial and nonfinancial incentives for clinicians to adopt accountable care.
Evaluation and Management
CMS is proposing to implement the complexity add-on code, HCPCS code G2211, beginning January 1, 2024. We appreciate that CMS is recognizing additional complexity inherent in the delivery of continuous, comprehensive, coordinated primary care, as well as other ongoing services, and taking steps to improve fair valuation and payment for these services under the MPFS. We support implementation of this code for CY 2024.
Additional Payment Changes
CMS make several proposals for physician payment which recognize the evolution of care delivery. NAACOS supports the following changes:
- Telehealth. In addition to implementing provisions of the Consolidated Appropriations Act of 2023, CMS proposes to add codes for health and well-being coaching services on a temporary basis and for social determinant of health (SDOH) risk assessments on a permanent basis to the Medicare Telehealth Services List effective January 1, 2024.
- Behavioral Health. CMS expands the types of providers that can deliver behavioral health services and increase the valuation for timed behavioral health services.
- Services addressing health-related social risk needs. CMS is proposing to pay separately for services that address health-related social needs (HRSNs), including community health integration services, principal illness navigation services, and SDOH risk assessment.
MEDICARE SHARED SAVINGS PROGRAM
Quality
NAACOS is pleased to see CMS proposals to introduce an additional reporting option, Medicare CQMs, to ease the transition to required electronic clinical quality measures (eCQMs) and Merit-Based Incentive Payment System clinical quality measures (MIPS CQMs) reporting for ACOs. We continue to have concerns regarding CMS’s larger goal to require all ACOs report all-payer eCQMs/MIPS CQMs, while making no changes to these reporting options. CMS notes this is intended to be a temporary, transitional reporting option. This will result in the same challenges being present for ACOs when the reporting option is eliminated because changes have not been made to the eCQM or MIPS CQM reporting options. The MSSP program-wide pay-for-performance implementation of eCQMs/MIPS CQMs should not move forward without proof-of-concept of both technical feasibility and the impact of the shift to all-payer measurement for ACOs. CMS must also consider future digital quality measurement (dQM) goals and how this proposal works to further that goal. ACOs should not have to invest in work-arounds now that will be obsolete in the near future as other technologies are introduced like Fast Healthcare Interoperability Resources (FHIR)-based Application Programming Interfaces (APIs).
NAACOS continues to have concerns the current state of data standards and interoperability will not yet fully enable ACOs to meet the eCQM reporting requirements successfully. While CMS and others often assume that electronic health record (EHR) vendors with 2015 Certified EHR Technology (CEHRT) would automatically include the capability to easily report the most recent version of an eCQM for MIPS with minimal manual effort, this is not the case. CEHRT requirements do not standardize the capture and reporting of individual eCQM data elements across vendor systems, and ACOs will need to tailor data extracts and uploads across systems and participating Tax Identification Numbers (TINs). Additionally, not all CEHRT vendors will implement every eCQM required for ACO reporting, since this is not a CEHRT requirement, potentially leaving a gap for ACOs. Additionally, this does policy does not advance digital quality measurement as it leaves the eCQM reporting option unchanged. Instead, CMS should make the proposed Medicare CQM changes (limiting the patient population) applicable to the eCQM reporting option as well and work with ACOs to ensure a more digital measurement approach will be feasible.
NAACOS continues to have concerns with CMS’s timeline to sunset the Web Interface reporting method for performance year (PY) 2025. Moving to more digital measurement that is bidirectional and improves clinicians’ ability to improve patient care at the point of care is a laudable goal. However, CMS must have realistic timelines when placing requirements on industry. According to a poll of our membership, only 38 percent of ACOs responding said they will be able to report eCQMs in 2025. What’s more, this transition is very costly for many ACOs. Forty-one percent of those surveyed estimated a cost of $100,000 to $499,000 and 32 percent estimated more than $500,000 to achieve eCQM requirements for the first year of reporting. Further, many vendors continue to tell ACO clients they are unable to support this work at this time.
As a result, CMS should instead view the Medicare CQM option as a permanent option that is in place until digital quality measurement and reporting is feasible for all ACOs. We continue to believe CMS should pilot eCQMs and dQMs for a subset of ACOs who feel best suited to move forward to identify key challenges and unintended consequences that need to be resolved before moving forward on a program-wide basis. Additionally, CMS should provide incentives for ACOs to do this testing, such as providing pay-for-reporting status for quality measures, upfront funding, adjustments to financial benchmarks, or an increased savings rate to help offset the high costs for doing this work.
Medicare CQMs
NAACOS applauds CMS for being responsive to several key concerns raised by NAACOS and ACOs regarding feasibility of implementing eCQMs and MIPS CQMs through its proposal to include a new reporting option, Medicare CQMs for MSSP ACOs. Limiting quality reporting to Medicare patients instead of all payer data eliminates concerns regarding equity. Additionally, further limiting the definition of a beneficiary eligible for Medicare CQMs to those meeting ACO assignment criteria mitigates concerns with specialists reporting on primary care focused measures included in the ACO measure set. However, because these policy changes are limited to the Medicare CQM reporting type and CMS is maintaining the eCQM reporting option with no changes, we remain concerned that the issues we have raised remain as the Medicare CQM option is designed to be a time limited option. As stated above, CMS should view the Medicare CQM option as a permanent reporting option that is in place until digital quality measurement and reporting is feasible for all ACOs.
Additionally, we urge CMS to limit reporting of Medicare CQMs to the patient list provided by CMS at the start of the reporting period. CMS notes it will not have full claims run-out information at the time of issuing this list, and therefore it will be incumbent on ACOs to ensure the list is complete. This adds significant burden and instead CMS should limit reporting of Medicare CQMs to the patients included on the list issued by CMS to ACOs reporting Medicare CQMs.
Timeline and Availability of Medicare CQMs
NAACOS has concerns that ACOs and their vendors will not be ready to support reporting with the new Medicare CQM option for the 2024 performance year. Identifying patients meeting the newly proposed criteria for Medicare CQMs will take time, and in order for ACOs to make investments in this new option CMS must signal Medicare CQMs will be available as an option for the foreseeable future. Reporting Medicare CQMs will still take significant resources and time for ACOs doing complex data aggregation and patient matching across many TINs and EHR types. We urge CMS to limit reporting of Medicare CQMs to the patients provided on the CMS-issued list at the beginning of the reporting period, as this would reduce the burden associated with reporting significantly and make the option a more feasible one for 2024.
Data Completeness
NAACOS urges CMS to clarify what the data completeness requirement for Medicare CQMs is, as the regulation discusses a 75 percent data completeness requirement and also notes CMS expects ACOs to report on all patients meeting the Medicare CQM eligibility criteria that also meet the measure criteria. It is not practical to expect ACOs to have 100 percent complete data when aggregating data across many practices, EHRs and instances of EHRs sometimes for both employed and independent clinicians. We urge CMS to adopt exclusions and/or a lower data completeness requirement for ACOs to account for these very real obstacles ACOs are working to overcome when reporting data to CMS for eCQMs, MIPS CQMs and Medicare CQMs when reporting at the ACO level. Other reporting methods began with a lower data completeness standard that then increased over time. Particularly with the eCQM, MIPS CQM and Medicare CQM reporting types having a much a higher burden than reporting of the Web Interface, we urge CMS to consider a data completeness standard lower than 75 percent. NAACOS opposes any increases in the data completeness standard for ACOs and asks CMS to consider what their goals for this requirement are, particularly in the context of ACOs reporting eCQMs, MIPS CQMs and Medicare CQMs.
Benchmarks
For the first year Medicare CQMs are made available (PY 2024) we urge CMS to consider using Web Interface benchmarks. Not knowing what benchmarks will look like prior to the start of the performance year will discourage ACOs from using the option. ACOs must have some level of certainty regarding what their quality targets will be prior to selecting a reporting option. We also ask CMS to clarify how they will handle developing a benchmark if less than 20 ACOs choose to use this reporting option.
On review of the existing benchmarking process for MIPS CQMs, eCQMs, and now Medicare CQMs, we do not believe that the process for distributing performance across deciles is transparent nor does this approach as constructed produce information that is meaningful. For example, the current process of determining whether a benchmark can be created appears to be arbitrarily set based on 20 entities reporting at least 20 patients in the denominator, which may or may not yield reliable results. There is also a significant risk of variation and instability in the benchmarks from year to year that may be due to changes in the number of entities reporting on a measure or other random variation rather than representing true differences in performance. The approach also assumes that all measures should be scored with the potential to achieve 100% (or 0% if it is an inverse measure) and while it may be a laudable goal, it may not reflect clinical knowledge or practical considerations of quality.
CMS must revise these methodologies for MIPS CQMs, eCQMs, and Medicare CQMs to increase transparency, consider the impact of random fluctuation, and be adjusted for practical considerations of comparison and relative performance. CMS could consider a process similar to the recent benchmarking of the Web Interface measures where thresholds are not dependent on random fluctuations in performance or because a measure is new to the program, rather they would be defined based on pre-determined distributions of performance. This approach would ensure that the benchmarking process is transparent and predictable and enable ACOs to participate in the program in a more meaningful way.
Changes to the Quality Performance Standard
We continue to believe tying ACO quality performance thresholds to MIPS scores is inappropriate and makes unfair comparisons. However, in the context of what has been proposed NAACOS supports CMS proposed changes to the MSSP Quality Performance Standard (QPS) calculations to move to a three-year average of historic performance data with a one-year lag for calculating the QPS. This proposal will provide ACOs with more certainty regarding what quality targets are in advance of the performance period starting and mitigate the potential impact of annual program changes affecting the QPS scores. We reiterate our request to have CMS publish MIPS quality performance category scores in the Public Use Files to bring greater transparency to these calculations.
Proposal to Apply a Shared Savings Program Scoring Policy for Excluded/Suppressed APP Measures
NAACOS supports CMS proposals to apply an MSSP specific policy for measures suppressed from quality scoring, providing ACOs with the higher of their own score or the QPS if a measure is suppressed for a performance year. These changes will ensure ACOs are not negatively impacted by measure changes or benchmark issues that occur mid-year and are outside the ACO’s control
ACO Quality Measure Changes
NAACOS supports CMS’s efforts to align quality measures across its programs by using the new Universal Foundation measure set, however we caution CMS to balance alignment with efforts to reduce administrative burdens. Should CMS continue to refine the Universal Foundation measure set, it must ensure there is not significant growth in the number of measures ACOs must report. CMS started the MSSP with over 30 quality measures, and over time reduced the measure set to reduce burdens associated with reporting. This should continue to be a focus for CMS. We also urge CMS to first test measures before making them required and scored measures for ACOs. Finally, NAACOS cautions CMS from implementing multiple major changes to the measure set in PY 2025 as this is the year the Web Interface is currently scheduled to sunset as a reporting option for ACOs, particularly as ACOs will now also be considering and preparing for a new reporting option (Medicare CQMs).
CMS should not require reporting on substance use disorder (SUD) treatment, until they are able to share SUD information with ACOs, as this is currently suppressed from data shared with ACOs for care coordination activities. Regarding the screening for SDOH measure, we caution this measure must be tested before making this a required measure. NAACOS supports CMS efforts to improve health inequities and incentivize screenings for social drivers of health. However, CMS must recognize the current state of this work and first start with efforts around data standardization before any such measures are required in performance-based programs like the MSSP. This work is iterative, and we are still in the early phases, therefore CMS should limit any measures on social drivers of health screening to optional measures, or if required, provide pay-for-reporting for these measures within ACOs to allow more learning to happen in this space. CMS should also allow for more standardization to occur and to gather data and learn about workflow issues that occur with screenings during a testing/pilot phase where any screening measure would be pay-for-reporting and would not dictate which screening tool was used, or how it was implemented. As an example, some ACOs may choose to do the screening as part of an office visit while others may instead find more value in providing an online screening tool that is completed outside an office visit. Regardless, screening measures should be used as one tool in a larger plan to address health inequities and provide high value care to underserved communities. Further, CMS is currently requiring collection of this data across multiple setting-specific programs, which could result in duplicative efforts and patients potentially having to share this information numerous times. CMS should explore how this data can be shared across providers. NAACOS has provided detailed recommendations on this topic, including more impactful ways CMS could engage with ACOs on this issue. Lastly, we point out that these measures are currently only available for one reporting type and question the feasibility of adding them to the measure set for ACOs.
Beneficiary Assignment
Modifications to Assignment Methodology and Identification of Assignable Beneficiary Population
NAACOS appreciates CMS’s efforts to eliminate barriers for beneficiaries to be assigned to ACOs. CMS proposes several changes to the assignment methodology, including revising the physician pre-step, implementing an expanded window for assignment, adding a third step to the claims-based assignment methodology, and revising the definition of assignable beneficiary. We support the overall goal to expand access to accountable care, particularly for beneficiaries in rural and other areas experiencing primary care physician shortages. Given the numerous program operations that rely on the assignable and assigned beneficiary populations, we urge CMS to conduct additional analyses including more years of data to ensure the changes do not have unintended consequences for certain types of ACOs or those operating in particular regions such as rural ACOs.
Use of an Expanded Window for Assignment
NAACOS supports the proposal to define “expanded window for assignment” as the 24-month period that includes the applicable 12-month assignment window and the preceding 12 months, as this appropriately aligns the expanded window for assignment with the different 12-month assignment windows used by ACOs operating under prospective assignment versus preliminary prospective assignment with retrospective reconciliation.
NAACOS supports efforts to better account for beneficiaries who primarily receive primary care services from non-physician practitioners (NPPs) during the assignment window and who received a primary care service from a physician during the expanded window for assignment. However, we believe CMS needs to establish a more refined approach for defining primary care delivered by these provider types before moving forward. We agree with CMS that the current approaches create challenges for NPPs, including nurse practitioners (NPs), physician assistants (PAs), and clinical nurse specialists (CNSs), to drive assignment in MSSP ACOs. This can be particularly challenging for ACOs that rely heavily on NPPs to deliver coordinated, team-based primary care and struggle to attribute patients as a result. However, we are concerned that the lack of specialty designation for NPPs will lead to more specialty-driven assignment from these provider types. While the majority of NPPs practice in primary care settings, we increasingly see more NPPs working in specialty practices, often providing follow up care after an acute event such as a transplant. Because CMS does not have specialty designations for NPPs and classifies them all as primary care clinicians, this type of follow up care delivered by NPPs in specialty practices can lead to beneficiaries being attributed to an ACO with which they have no primary care relationship. ACOs report that beneficiaries aligning through specialists in this way tend to be those who are receiving a high-cost procedure in the performance year and do not align to the ACO again in future performance years, making it challenging for ACOs to meet their benchmarks.
CMS should investigate the impacts of specialty-driven assignment, including differences in risk scores and costs for beneficiaries attributed via specialists to inform future policy solutions. For example, if data show that these beneficiaries have higher risk scores and higher costs, there could be opportunities to address these challenges through benchmarking and risk adjustment policies. Attribution churn is another area with opportunity for improvement. ACOs struggle to maintain attribution for beneficiaries attributed through specialists because they do not have a primary care relationship with the ACO. CMS should explore strategies to support ACOs in leveraging specialty-driven assignment through NPPs to develop longitudinal primary care relationships with these beneficiaries and advance the goal of having all beneficiaries in an accountable care relationship by 2030.
While these proposals mitigate some of these concerns by retaining the requirement for a physician visit in the 12 months preceding the assignment window, the fundamental issue of not identifying NPPs as primary care clinicians or specialists remains. ACOs are differentially impacted by this depending on the ACO’s composition. ACOs including large multispecialty practices or academic medical centers experience more specialist-driven attribution related to care delivered by NPPs in these settings. As our health care system continues to shift to value-based payment and accountable care, it’s important to understand the care that’s being provided so that we can better manage and appropriately pay for that care.
Solutions include updating the Provider Enrollment, Chain, and Ownership System (PECOS) to include specialty designations for NPPs. CMS could begin by collecting this information as an optional field in the Medicare enrollment application, which already includes this field for physicians. This would provide more information about the type of care being provided by NPPs and enable CMS to align beneficiaries more accurately with their primary care clinicians. Allowing participation at the TIN-National Provider Identifier (NPI) level in MSSP, as opposed to full-TIN participation, would also alleviate these concerns. ACOs in Innovation Center models, like ACO REACH and the Next Generation ACO Model, define participation at the TIN-NPI level and as such, can exclude specialty-focused NPPs from driving assignment. We believe NPPs that deliver primary care, as opposed to specialty care, should play a prominent role in ACO assignment. In the absence of CMS’s ability to distinguish between NPPs who practice primary care and those who practice specialty care, we continue to advocate that ACOs be permitted to remove specialty focused NPPs from assignment.
Addition of a Step Three to the Assignment Methodology
NAACOs supports CMS’s proposals to add a new step three to the claims-based assignment methodology utilizing the expanded window for assignment to identify beneficiaries currently excluded from assignment under the existing pre-step. We appreciate CMS applying this step after the current methodology to ensure that all beneficiaries who are assigned to an ACO under the current methodology would continue to be assigned to an ACO. CMS notes in its proposals that there may be a share of beneficiaries who would be prospectively assigned to an ACO under the proposed step three that differs from the retrospective ACO the beneficiary is assigned to under the current methodology. While this will likely affect a small number of beneficiaries, we encourage CMS to monitor these shifts to ensure ACOs operating under retrospective assignment, particularly small and rural ACOs, are not unduly disadvantaged by these policies.
Revision of the Definition of Assignable Beneficiary
NAACOS strongly urges CMS to conduct further analyses using additional years of data prior to revising the definition of an assignable beneficiary to align with the proposed expanded window for assignment. We appreciate that under CMS’s proposals, all beneficiaries who are currently assignable would continue to be assignable and that beneficiaries who do not receive any primary care services during the assignment window would continue to be excluded from the assignable population. However, due to the numerous program operations that rely on the national and regional assignable populations and the potential impacts to financial calculations, more information is needed to determine whether this is good policy.
The simulation of changes to the national assignable population provided in Table 30 only relies on one year of data, PY 2021, which was impacted by anomalies related to the COVID-19 pandemic. CMS should expand this simulation to include additional data years (e.g., 2019, 2020, 2021, and 2022). While CMS estimates that the overall growth in the national assignable population will be small (about 2.9 percent), it does not examine changes to regional assignable populations, which are used in calculations to adjust ACOs’ financial benchmarks. We are concerned that rural ACOs could see more significant changes to regional adjustment factors due to smaller population sizes. Because CMS proposes to adjust benchmarks for all ACOs, regardless of agreement start date, based on the new assignment methodology and definition of assignable beneficiary, the agency risks harming current ACOs that may be disadvantaged under the new policies.
NAACOS recommends that CMS expand on the simulation and provide additional analyses to assess:
- Impacts to individual ACO benchmarks to ensure the policies do not harm performance and create artificial winners and losers,
- Potential changes to regional factors calculated with the new regional assignable population to ensure there are not unintended consequences for rural ACOs and ACOs in underserved communities,
- Changes to PBPY expenditures and average risk scores under the new assignable definition, and
- Differential impacts based on geography, ACO size and composition, and between retrospective ACOs and prospective ACOs.
Revisions to the Definition of Primary Care Services Used in Assignment
CMS proposes to add several codes to the definition of primary care services used to determine beneficiary assignment. NAACOS supports the addition of the following codes:
- Smoking and Tobacco-use Cessation Counseling Services (CPT codes 99406, 99407)
- Cervical or Vaginal Cancer Screening (HCPCS code G0101)
- Complex E/M Services Add-on (HCPCS code G2211)
- Community Health Integration Services (HCPCS codes GXXX1, GXXX2)
- Principal Illness Navigation Services (HCPCS codes GXXX3, GXXX4)
- SDOH Risk Assessment (HCPCS code GXXX5)
- Caregiver Behavior Management Training (CPT codes 96202, 96203)
- Caregiver Training Services (CPT codes 9X015, 9X016, 9X017)
We believe these services support the delivery of comprehensive, coordinated, whole-person primary care and encourage CMS to finalize their addition to the definition of primary care services as proposed.
CMS also proposes to add Remote Physiologic Monitoring Treatment Management Services (CPT codes 99457, 99458). While these codes may be billed by primary care providers to support the overall management of a patient’s care, the codes can also be billed by specialists and importantly, can only be billed by one treating provider for a given patient. Therefore, if a specialist is billing these codes to support management of a specific condition, that patient’s primary care provider would not be able to also provide RPM treatment management services to the patient. Further, because these are monthly billable codes, this could result in the allowed charges for RPM services furnished by a specialist surpassing the allowed charges for primary care services furnished by the PCP. NAACOS supports the addition of these codes, as we believe they support comprehensive care management, but we encourage CMS to monitor billing of the codes to ensure their addition is not shifting beneficiary attribution away from primary care relationships in favor of specialty care.
Finally, CMS proposes to add Office-Based Opioid Use Disorder (OUD) Services (HCPCS codes G2086, G2087, G2088). CMS notes in its proposal that it excludes these codes from CCLFs provided to ACOs and ACOs would not be able see these claims or identify why certain beneficiaries were assigned to their ACO related to these codes. NAACOS opposes the addition of these codes to the definition of primary care services used in assignment until CMS provides this information to ACOs. Despite the fact that Section 3221 of the Coronavirus Aid, Relief, and Economic Security (CARES) Act helped to align 42 CFR Part 2 (Part 2) with HIPAA, ACOs still lack access to vital SUD-related data on their patients due to the fact that under current regulations, care coordination is not considered by CMS to fall under treatment, payment, and health care operations. By aligning Part 2 with HIPAA, the CARES Act allows sharing of this important data after initial patient consent, which will allow CMS to deliver this critical information to providers operating in ACOs. NAACOS continues to advocate for CMS to provide timely, actionable data, including SUD-related data, to ACOs. ACOs rely on data to understand the full spectrum of a patient’s care needs and inform evidence-based treatment. Without access to such claims data, ACOs risk treating the whole patient with only part of their data, potentially harming patient care and outcomes.
Benchmarking Methodology
NAACOS appreciates CMS’s commitment to ensuring ACOs are granted fairer, more accurate financial benchmarks, which we have long advocated for. Overall, proposals in this rule, if finalized, will help entice more providers to join the MSSP and keep others in the program. These proposed changes won’t help all ACOs but will help level the playing field for those who serve more at-risk, medically complex, or high-cost populations.
However, NAACOS cautions CMS that nothing in this proposed rule will solve the ratchet effect, where ACO benchmarks will continue to be lower over time as they reduce spending in their populations and future benchmarks are rebased on lower historic spending. NAACOS implores CMS to consider future changes to mitigate this rebasing problem, which we believe threatens future participation for ACOs working to create a higher quality, more efficient, and more cost-effective health system. More dramatic benchmarking policies are needed to both attract new participants while keeping existing ACOs in the model.
Additionally, CMS’s high-low revenue distinction is continuing to hurt providers who serve vulnerable populations, including rural and safety-net providers. Evaluations show that ACOs with federally qualified health centers (FQHCs), rural health clinics (RHCs), and critical access hospitals (CAHs) as participants are more likely to be classified as high revenue and therefore would be disqualified from receiving some program benefits such as the Advance Investment Payments. In 2020, 71 percent of low-revenue ACOs did not include a FQHC, RHC or CAH. Conversely, 46 percent of high revenue ACOs included 5 or more FQHCs, RHCs, or CAHs. CMS should instead consider alternative approaches, such as evaluating the demographics of the population served by an ACO. The high/low revenue status is arbitrary and leaves out the very ACOs CMS is trying to attract to the program.
Lastly, CMS needs to take action to correct an impending issue around drugs in the 340B program. Since a Supreme Court decision last year, CMS has not addressed the disparity between ACOs who paid for 340B drugs at lower prices during their benchmark years and at higher prices during their performance years. This will continue to hurt ACOs that have 2018-2022 in any of their baseline years for benchmarks. We urge CMS to correct this disparity by adjusting its calculation of ACOs’ performance year expenditures to correct for this difference in 340B drugs without ACOs having to early renew. This adjustment would help ACOs with 340B providers, who help under-served patients and address the health disparities CMS wants to eliminate.
Capping Reginal Risk Score Growth
CMS proposes to cap an ACO region’s growth in risk scores at 3 percent, similar to how it caps the ACO’s own risk score growth. CMS proposes to apply the cap on the region independently, meaning the region could be subject to a cap in its risk scores even if the ACO isn’t. ACOs in regions with risk score growth below the cap would not be affected. The cap for both the ACO and region is applied separately for each enrollment type. If finalized, the change would apply to new agreements starting in 2024.
NAACOS supports this change and thanks CMS for listening to our concerns. We have been advocating for a very similar policy. This will incentivize ACO participation in regions with high risk scores and encourage ACOs to care for higher risk beneficiaries. As CMS estimates, 11 percent of ACOs in 2021 would have benefited from this proposed change, a number that would increase as ACOs get further along in their 5-year agreement periods and would be more likely to hit the 3 percent cap. As with all these changes to the financial methodology, we encourage CMS to apply this change to all ACOs, not just new agreements.
Eliminating the Negative Regional Adjustment
CMS proposes to prevent any ACO from receiving a regional adjustment that would cause its benchmark to be lower than it would have been without the regional adjustment, effectively eliminating the negative regional adjustment. ACOs eligible for a prior savings adjustment would not have those savings offset by a negative regional adjustment. If finalized, this change would take effect for new agreements starting in 2024.
NAACOS supports this change as it would remove the disincentive for ACOs with spending higher than their region to participate in MSSP. However, we urge CMS to apply this change to all ACOs, not just those starting new agreements in 2024. While NAACOS understands the reasoning behind the negative regional adjustment, it harms ACOs whose patients are costlier and can work against CMS’s health equity goals by shunning providers who serve sicker, possibility more medically complex populations. As CMS notes in the rule, ACOs who receive a negative adjustment are twice as likely to drop out of MSSP.
While there’s no proposed change for ACOs with a positive regional adjustment, NAACOS reiterates its stance on needing to provide additional help to ACOs who have already lowered costs in their communities. This includes ACOs who receive the full positive regional adjustment or max out their prior savings adjustment. There is effectively a cap on ACOs’ savings under these current policies, which should be addressed if CMS wishes to have successful ACOs remain in MSSP. Any cap on savings does not exist in other Medicare programs, including Medicare Advantage.
Modifying the Prior Savings Adjustment
CMS proposes to recalculate an ACO’s prior savings adjustment if shared saving amounts are retroactively adjusted to account for either 1) compliance actions to address an avoidance of at-risk beneficiaries or 2) a redetermination of shared savings or losses. NAACOS supports this change as it increases program integrity without implementing undue burden on ACOS.
Introduction of New Risk Adjustment Model Version
For new agreements beginning in 2024, CMS proposes to use the same hierarchical condition code (HCC) risk adjustment model for a performance year and the relevant benchmark years. This means that as CMS introduces new risk models, including the forthcoming V28, risk scores would be calculated using a consistent model and any impacts a shift in the model version could create should be balanced. Importantly, these changes will only apply for agreement periods beginning in 2024 with CMS saying it historically incorporates changes to the benchmarking methodology at the start of an ACO’s agreement period. ACOs not starting new agreements in 2024 will have risk scores for their benchmark years calculated using different HCC model versions.
Mirroring risk model between benchmark years and performance years
NAACOS supports CMS using a consistent risk model in both the performance and all benchmark years. We urge CMS in the final rule to apply a consistent risk model for all ACOs, not just those starting new agreement periods next year. Using a consistent risk model creates a fair, apples-to-apples comparison in MSSP’s risk adjustment methodology, which compares patient populations’ risk scores between a baseline period and the relevant performance year. Using different HCC model versions between these two sets of years creates a fundamentally flawed comparison. This is especially true given the changes seen between V28 and V24, which collapses a large number of codes and revalues many others. Even if ACOs have the same patient populations with the same level of sickness, HCC scores will be lower under the new V28 model. Additionally:
- CMS noted in its proposed rule, ACOs would be hurt by using inconsistent risk models between benchmark and performance years. ACO shared saving payments would have been 11 percent lower in 2021 with inconsistent models. This compares to shared savings payments being 2 percent higher that year if V28 were used in both the performance and benchmark years.
- Similarly, a NAACOS’ analysis demonstrated that dual eligible and disabled beneficiaries would be disproportionately harmed by using the V28 model when the V24 model is used in the benchmark.
- ACOs were not aware of the impact of risk model changes prior to the deadline to early new—the proposed rule was published on July 13 and the deadline to submit application for new agreements was June 15.
- There’s precedence for CMS to apply adjustments to all ACOs, not just those starting new agreements. CMS does this annually with billing codes used in assignment and previously all policies for risk adjustment were not codified in regulations, allowing the agency to make subregulatory changes.
Blending of New Risk Model Versions
CMS proposes to phase in the new V28 risk model over a three-year period, similar to how it will for Medicare Advantage plans starting next year. This will apply to all MSSP ACOs, not just those starting new agreement periods.
NAACOS supports this change believing that introducing the new V28 risk model over a blended, three-year period is a fair way to incorporate the model into MSSP. Furthermore, it matches how CMS is implementing the model in other Medicare programs. NAACOS also appreciates that this blended introduction is done for all ACOs. We hope CMS could similarly apply other risk adjustment and benchmarking policies to all ACOs, not just those who are starting new agreements.
Codifying Risk Adjustment Policies
CMS will also codify its risk adjustment approach, which currently is missing from the regulations that govern the MSSP. NAACOS supports this and urges CMS to consider additional changes to MSSP risk adjustment policy. This includes rising the 3 percent cap on ACOs’ risk scores but also alternatives that eliminate providers’ emphasis on collecting patient diagnoses for the purposes of increasing risk scores. The burden of collecting codes for risk adjustment is onerous and has become a burden on ACOs. It’s time to consider a new paradigm that moves away from this risk-coding game. If an ACO is only successful by increasing risk capture, then we’re losing our principles of improving care and reducing unnecessary utilization.
Alternatives include replacing the current 3 percent cap on scores with the possibility of risk adjustment audits, which are currently in place for Medicare Advantage plans. Additionally, CMS should monitor if the move to the V28 model will modify incentives to collect patient risk. CMS could install a cap on risk scores decreasing, which currently doesn’t exist. Relatedly, we ask CMS conduct analysis on the effect of the cap on years later in a five-year agreement period.
Advance Investment Payments Policies
NAACOS was pleased to see CMS establish the advance investment payments (AIP) option in MSSP through last year’s rulemaking, as we have long advocated for CMS to make upfront funding available to ACOs. NAACOS appreciates CMS making refinements and clarifications to AIP policies in advance of implementation beginning January 1, 2024. We share CMS’s commitment to supporting the provision of accountable care for underserved beneficiaries and encourage CMS finalize, with modifications, the proposals as detailed below.
AIP Eligibility Requirements
We appreciate CMS’s recognition that ACOs vary in their ability to take on downside risk in this proposal to allow ACOs to progress to two-sided risk along the Basic Track’s glide path after the second performance year within an agreement period in which AIPs are received. NAACOS supports this proposal, and we encourage CMS to explore other options to expand eligibility criteria for AIP to ensure equitable access to accountable care for all beneficiaries. As described in previous comments, the current eligibility criteria are overly limiting and exclude many FQHCs, RHC, CAHs, and other crucial safety net providers from receiving AIP, as they are often designated as high revenue by CMS’s definition despite having limited access to capital to invest in ACO activities. Additionally, many existing ACOs, including those that are designated as experienced with performance-based risk or participating in the Enhanced Track, still lack the significant resources and infrastructure required to meaningfully address patients’ SDOH and HRSNs. AIP could be leveraged by these ACOs to enhance sociodemographic data collection, create targeted initiatives to reduce health disparities, and develop relationships with community-based organizations (CBOs) to address social needs. As the AIP program is rolled out, CMS should assess how the funds are used and consider expanding these criteria further to include more types of ACOs and diverse provider types so that more patients can benefit from these important investments.
AIP Recoupment and Recovery Policies
In this proposal, CMS acknowledges it did not address the interactions between AIP recovery policies and a voluntary termination of the participation agreement by an ACO that is seeking to early renew. To address this, CMS proposes to create an exception to the recovery policy for an ACO that voluntarily terminates its participation agreement at the end of PY2 or later provided the ACO immediately enters a new participation agreement under any level of the Basic Track or the Enhanced Track. Under this exception, the ACO would not be required to immediately repay all AIPs received following notice of termination and would rather have the AIP balance carried over to the new agreement period. NAACOS supports this proposal, and we agree that ACOs should have the flexibility to participate in MSSP in the manner that works best for their structure and patient population. We appreciate CMS providing ACOs the flexibility to enter a new agreement period to experience MSSP policy changes that are only applicable to new agreements without having to immediately pay back the AIP funds they received.
We also support the proposal to allow ACOs that receive AIP and opt to early renew to spend the AIP funds in their second agreement period provided the funds are spent within 5 performance years.
As detailed in past comments, NAACOS recommends CMS further modify AIP recoupment and recovery policies to encourage continued participation in MSSP and consider ACOs’ need for sustainable funding. Under current policies, CMS will recoup AIP from any shared savings earned by an ACO until all AIP funds are repaid. As such, many ACOs may not receive shared savings payments for a significant period of time, which could discourage continued participation. While receipt of AIP will help stand up initial ACO infrastructure and activities, annual shared savings payments are crucial to fund sustained initiatives and continual improvement. We recommend CMS recoup AIP funds from a portion of shared savings earned by the ACO so the ACO can fund ongoing initiatives.
Termination Policies
CMS proposes to amend AIP termination policies to allow CMS to cease distribution of AIP following an ACO’s notice of voluntary termination (if the ACO will not early renew), to be consistent with the policy to cease distribution if an ACO fails to comply with the requirements of § 425.630 or meets any of the grounds for termination under § 425.218(b). NAACOS supports this proposal as it avoids distribution of funds that would need to be immediately repaid.
More broadly, we believe CMS should account for investments with continuing benefits in termination and recovery policies. NAACOS suggests CMS consider an ACO’s circumstances and timing of termination, in addition to the investments made with the funds, rather than immediately require all spent and unspent AIP funds be repaid. For example, if an ACO spent AIP funds on EHR upgrades in the initial years of the participation agreement and had to terminate in year four or five, those investments would continue to benefit Medicare beneficiaries and providers even absent the ACO’s continued participation in MSSP. We recommend CMS modify termination and recovery policies to take a more thoughtful approach.
Reporting Requirements
Current AIP policies require ACOs receiving AIP to publicly report the ACO’s spend plan, the total amount of AIP funds received, and an itemization of how AIP funds were spent during the performance year. CMS proposes to require that ACOs report this information to CMS as well. NAACOS supports this proposal, and we appreciate that the agency will use the submitted data as the template that ACOs can use to populate their public reporting webpages, as this should minimize administrative burden. We encourage CMS to provide any feedback on the data submitted by ACOs with enough time to make any needed changes prior to publicly reporting.
Reconsideration Review
CMS proposes to allow an ACO receiving AIP to request reconsideration review of all quarterly payment calculations, rather than only when CMS calculates that no payment will be made. NAACOS supports this proposal. We encourage CMS to provide payment calculation details far enough in advance to allow time to resolve reconsiderations and avoid delayed payments to the ACO.
Eligibility Requirements
Shared Governance Requirement
Current AIP policies require ACOs receiving AIP to publicly report the ACO’s spend plan, the total amount of AIP funds received, and an itemization of how AIP funds were spent during the performance year. CMS proposes to require that ACOs report this information to CMS as well. NAACOS supports this proposal, and we appreciate that the agency will use the submitted data as the template that ACOs can use to populate their public reporting webpages, as this should minimize administrative burden. We encourage CMS to provide any feedback on the data submitted by ACOs with enough time to make any needed changes prior to publicly reporting.
Identifying ACOs Experienced with Risk Based on TINs’ Prior Participation
CMS proposes to codify the agency’s current operational approach for determining whether an ACO participant TIN has “participated” in a performance-based risk Medicare ACO initiative. CMS proposes to modify the existing definitions for “experienced with performance-based risk Medicare ACO initiatives” and “inexperienced with performance-based risk Medicare ACO initiatives” to include the language, “An ACO participant is considered to have participated in a performance-based risk Medicare ACO initiative if the ACO participant TIN was or will be included in financial reconciliation for a performance year under such initiative during any of the 5 most recent performance years.”
NAACOS supports this proposal, and we appreciate CMS’s transparency with program operations. To define participation accurately and fairly, we encourage CMS to establish a process whereby ACOs may request reconsideration review if an ACO participant TIN is considered to have participated in an Innovation Center ACO model when only a small proportion of NPIs billing under the TIN participated in the model demonstration. Given MSSP is a full-TIN model and many CMMI models are under “split-TIN” or TIN-NPI participation, it is reasonable to utilize a threshold to determine participation for a TIN which had a portion of NPIs participating in a CMMI ACO model. CMS could use the threshold that is currently in place for the ACO-level experience criteria and consider a TIN to have participated if forty percent or more of the NPIs billing under the TIN were included in the model participant list.
Technical Changes
NAACOS supports the following proposals to make technical changes to references in MSSP regulations, which will eliminate existing errors and inconsistencies and improve clarity in the regulatory text:
- Revise references to an ACO’s assignment methodology selection to eliminate inconsistencies between the use of § 425.226 (which describes actions for which an ACO is responsible in selecting and changing its selection of assignment methodology) and § 425.400 (which outlines how CMS employs the assignment methodology for program operations).
- Correct the definition of “RHC” by replacing the word “center” with the word “clinic” and clarify that all uses of the acronym “RHC(s)” have been interpreted to refer to “rural health clinic(s).”
- Correct typographical errors in the definition of “at-risk beneficiary” by replacing the word “Medicaid” in paragraph (7) with the word “Medicare.”
- Update terminology in regulations on data sharing with ACOs by replacing references to “Health Insurance Claim Number (HICN),” which was discontinued in 2019, with the term “beneficiary identifier,” and revising the list of purposes for which an ACO may request certain beneficiary-identifiable data to replace the term “process development” with “protocol development.”
Future Developments for Shared Savings Program
NAACOS has advocated that CMS leverage MSSP as an innovation platform and applaud CMS for seeking input on ways to bring more innovation into the program. Additionally, NAACOS is pleased to see CMS mention an option to provide prospective payment for primary care within MSSP as a strategy to support care delivery transformation, strengthen primary care, and increase participation in ACO initiatives. NAACOS and others have called on CMS to implement such an option and outlined payment approaches that accommodate the differing needs and capabilities of various primary care practice types. We encourage CMS to move forward swiftly and begin offering this option in MSSP to coincide with the start of the Innovation Center’s Making Care Primary Model.
Incorporating a Higher Risk Track than Enhanced
CMS seeks feedback on, but did not propose, creating another track in the MSSP that offers higher levels of risk and reward than the current Enhanced Track. NAACOS has advocated for such an option, which we’ve called “Enhanced Plus.” Such an option would encourage ACOs to take on higher levels of risk, which would in turn produce higher savings, drive innovation, and improve patient care overall. Accordingly, NAACOS was extremely pleased to see CMS request stakeholder feedback on a potential MSSP track that offers a higher level of risk than the current Enhanced track.
Our concept for “Enhanced Plus” would offer a bridge between Enhanced and what today is ACO REACH, all while providing more flexibility and innovation that allow providers to deliver optimal patient care in ways that best suit them and their populations. Now is an appropriate time for CMS to consider an Enhanced Plus option. With ACO REACH scheduled to sunset at the end of 2026, there’s growing uncertainty around what model is next for REACH ACOs. An Enhanced Plus option could provide an on-ramp to MSSP, which was lacking when Next Gen expired at the end of 2021. Below our recommendations offer approaches that would encourage adoption of a risk track higher than Enhanced by ACOs currently in MSSP or REACH.
First, CMS should give ACOs a choice between a full-risk option with a discount or a shared savings rate of 85 percent or 90 percent. There is precedence as ACO REACH offers two levels of risk and Next Gen offered options for percent shared savings (80 or 100), variable discounts, and caps on savings and loss rates between 5 percent and 15 percent. These options provide a tradeoff between how much ACOs could pay back to the Medicare trust fund or reinvest in incentives or patient care.
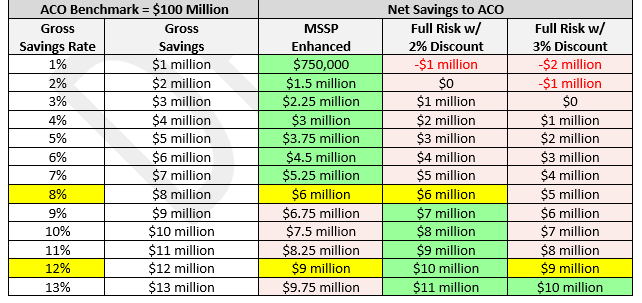
These varied approaches are needed to consider the financial incentives for ACOs. For example, the chart below demonstrates potential financial incentives under Enhanced and a theoretical Enhanced Plus. Today, the Enhanced track offers a 75 percent shared savings rate and a 40 percent shared loss rate. In a full-risk model with either a 2 percent or 3 percent discount, ACOs would have to generate savings of 8 percent or 12 percent, respectively, to earn more than in Enhanced. We understand that CMS must balance savings to Medicare with incentives to attract providers in the model.
It will be critical for CMS to also consider non-financial incentives to entice participation in a full-risk model given the relative attractiveness of the current Enhanced model. Few ACOs can generate the levels of savings needed to make a full-risk model with a discount more attractive. The answer lies in waivers and other non-financial incentives, which we spell out below.
- NPI-level participation – Innovation Center models have been very attractive for ACOs comprised of large health system and multispecialty practices because of their ability to be more selective on participants than the full-TIN model participation of MSSP. An Enhanced Plus model should allow TIN/NPI participation to allow ACOS better select its participants.
- Regional-only benchmarking – Enhanced Plus should employ more innovative benchmarking solutions, including setting ACO spending targets based entirely on that of ACOs’ regions with no reliance on ACO participants’ historic spending or need for a prior savings adjustment. NAACOS has long advocated for this for this as it would provide a sustainable path to participation for ACOs whose spending is historically below that of its region.
- Options for Population-Based Payments – These payments, which were offered in Next Gen, allowed ACOs to enter negotiated payment arrangements with specialists and preferred providers, which is a concept not present today in MSSP. The provider received a reduction in claims in exchange for other compensation determined by the ACO, based on quality and other utilization and outcome metrics. This option could help improve specialist involvement in ACOs.
- Advanced Payment Option – Another innovative tool offered by ACO REACH allows providers to receive payment for non-primary care services and other payments not covered by capitation options. This offers a better cash flow for ACO services that have proven to be critical. It allows ACOs to pre-pay performance and not wait 18 months for shared savings to invest in care management and technology.
- More waivers and flexibilities – Waivers available today in MSSP have become increasingly stale. In contrast, Innovation Center models offer much better ways to meet patient needs. Enhanced Plus should offer more advanced waivers, including the post discharge home visit waiver, care management home visit waiver, tailored Part B cost sharing support, and others being tested under ACO REACH. ACOs should have maximum flexibility to determine how to implement the benefit.
- Better access to data – Managing populations requires access to data to understand your patients, their health, their needs and where they’re seeking care. Enhanced Plus should provide access to data dashboards that existed under Next Gen, which were well used and very appropriate.
- Paper-based voluntary alignment – ACO REACH’s paper-based voluntary alignment has been well utilized and helps ACOs better engage patients. We hope it could be deployed to MSSP to better engage patients.
In the RFI, CMS asked questions about how to protect the Medicare trust fund if only highly confident or successful ACOs joined a potential Enhanced Plus model or ACOs who may avoid high-cost patients. NAACOS believes there’s robust experience around risk corridors in Innovation Center models and a truncation factor in MSSP. Additionally, other aspects of ACO policy, such as benchmarks, risk adjustment and attribution, should be structured to ensure that ACOs can adequately care for high-cost patients.
CMS should expect highly confident and successful ACOs to join this new track. CMS’s aim should not be to attract unsuccessful ACOs but to ensure it designs a model that will generate savings to Medicare while providing ACOs with stable benchmarks and the flexibility to innovate and improve patient care. As an option, CMS could employ an early termination policy as was done in REACH to prevent ACOs from leaving the program before the end of their agreement period if the model became financially unfavorable for them.
NAACOS stands ready to work with CMS on developing more details around Enhanced Plus. We, however, caution CMS that it should still explore ways to offer successful waivers and innovations to ACOs in the Basic Track and Enhanced.
Increasing the Amount of the Prior Savings Adjustment
Regarding its calculation of the prior savings adjustment, CMS seeks comments on increasing the 50 percent scaling factor or other alternatives for measuring savings generated in a way that doesn’t overly inflate ACOs’ benchmarks while still reducing the ratchet effect. For contracts beginning in 2024, CMS previously finalized adding back half of ACOs’ prior savings to its benchmark, which cannot exceed 5 percent of national FFS spending, the same cap applied to an ACO’s positive regional adjustment.
NAACOS appreciates CMS’s openness to modifying prior savings adjustment. In our comments on last year’s fee schedule, we offered several ways to strengthen the prior savings adjustment.
- Use ACOs’ maximum shared savings rate from their prior agreement period. This would increase the prior savings adjustment to 75 percent for Enhanced ACOs, for example.
- Allow the prior savings adjustment to be more than 5 percent of national FFS spending, at which it is currently capped. The cap on the adjustment effectively limits successful ACOs’ or ACOs who serve high-costs population. For these ACOs, a cap of 5 percent may represent more than a 50 percent scaling factor of the prior contract’s savings.
- Risk adjust the 5 percent national FFS spending to make it a more accurate reflection of the complexity of the patient population.
- Allow ACOs to receive the greater of the 5 percent of national per capita FFS spending in BY3 for assignable beneficiaries or 50 percent of the pro-rated average per capita savings net of any negative regional adjustments.
- Use a quartile-based benchmark system, like Medicare Advantage, which would adjust the caps based on the ACOs’ spending compared to the region. For example, an ACO whose spending is 10 percent below their region could be capped at 5 percent while an ACO that is 20 percent below their region’s spending could be capped at 7.5 percent. Currently, CMS policy of ratcheting every ACO back to a 5 percent of national FFS spending prevents any long-term investments that would require greater than a 5 percent savings rate to generate a return.
NAACOS supports CMS’s efforts to account for prior savings when ACO benchmarks are rebased under a new agreement period as this will help CMS retain ACOs in the program long-term. NAACOS appreciates policies that reward strong performance and further incent a transition away from FFS. We feel there are ways to strengthen this policy that are important to consider as we deal with the ratchet effect that comes from continual rebasing. It’s important to remember that any move to administrative benchmarks won’t solve this problem of benchmarks starting off at unachievably low levels because of ratcheting due to rebasing. This ratchet does not just cap savings, it caps investments in beneficiaries, and it caps how much an ACO can truly transition away from FFS and towards value.
As CMS looks to solve the ratchet effect, it’s important to remember this could be solved by increasing both the regional adjustment and prior savings adjustment. The size of the ratchet depends on how efficient the region is, and ACOs in more efficient regions need a higher prior savings adjustment to offset the lack of help provided by the regional adjustment.
Expanding the ACPT Over Time and Addressing Overall Market-wide Ratchet Effects
CMS is seeking feedback on future refinements to its new Accountable Care Prospective Trend (ACPT), including replacing the national trend in the current two-way blended update with the ACPT, along with scaling the weight of the ACPT to account for ACOs’ market share in its region. NAACOS has expressed concern that the ACPT, because it’s based on national Medicare spending, would hurt ACOs in regions whose spending growth was higher than the ACPT. According to our analysis, that’s about a third of ACOs. For new agreements starting in 2024 and beyond, MSSP benchmarks will be a combination of two-thirds of the current national-regional blend rate and one-third of the ACPT.
NAACOS appreciates CMS looking at future refinements to the ACPT given our concerns with its implementation, which included calling for a pause on it starting in 2024. In last year’s rulemaking, we asked that CMS keep the current two-way trend that uses a blend of national and regional spending but recommended two changes: CMS (1) use the ACPT as the national component of the trend adjustment, rather than observed national FFS spending and (2) remove ACO-assigned beneficiaries from the regional comparison group, negating the effect of ACOs’ savings on the regional trend. This would still allow CMS to move toward its goal of an administratively set benchmark while minimizing the unintended consequences of harming nearly a third of ACOs.
Our concern with the ACPT hinges on the fact that national spending is not reflective of the spending trends in an ACO’s region. When an ACO’s regional trend is lower than national spending increases, the ACO would be negatively impacted. ACOs should not be punished if they operate in regions with spending growth below that of national inflation. Replacing the national trend in the current two-way blend with the ACPT is a step in the right direction. It creates a benchmark that is based less on national spending and more on regional spending, which is a policy NAACOS has long advocated for.
NAACOS continues to ask that guardrails be put into place to protect ACOs who would see lower benchmarks because of the ACPT. These include:
- Setting ACOs’ historic benchmark at the higher of the proposed three-way trend adjustment or the current two-way trend adjustment.
- Basing the ACPT on regional spending, rather than national. Because there is significant variation in regional spending growth, the use of a national trend will benefit ACOs in regions with slower spending growth and reduce benchmarks for ACOs in regions with higher spending growth.
- Using a 3-year projection of the ACPT, which is the current projection used in the USPCC. It would be difficult to project five years out, and reserving the right to make mid-agreement period adjustments simply introduces uncertainty.
Promoting ACO and CBO Collaboration
CMS seeks feedback on general approaches for encouraging or incentivizing increased collaboration between ACOs and CBOs and on potential changes to MSSP’s patient-centeredness requirements to strengthen partnerships between ACOs and interested parties in the community, including CBOs, to address unmet HRSNs. NAACOS shares CMS’s commitment to whole-person care, and we appreciate the opportunity to highlight ways to support ACOs in collaborating with CBOs and addressing health equity and SDOH. NAACOS has offered several recommended policy changes to support ACOs in this work, including increasing financial benchmarks for beneficiaries with social risk factors, providing funding for community partnerships, allowing additional flexibility for ACOs to provide supplemental benefits, leveraging technology, and providing ACOs timely access to data.
Many ACOs are actively working with their communities, by partnering with CBOs or implementing initiatives in partnership with local schools and churches to meet patients’ needs. A common barrier that ACOs encounter in this work is lack of funding and/or capacity of CBOs to meet the level of need in the community. Many CBOs across the country are small, underfunded, and lack connections to the health care system. While some ACOs use shared savings to fund partnerships with CBOs, more stable and predictable funding mechanisms are needed to create meaningful, sustained collaboration.
New codes for community health integration and SDOH risk assessment, proposed in this rule, will help support these efforts by providing payment for screening patients for SDOH and social risk factors, and for activities to address SDOH and HRSNs. We encourage CMS to do more to incorporate social risk into financial benchmarks to reflect the cost of improving outcomes more accurately for beneficiaries affected by SDOH and HRSNs. These beneficiaries may have significant unmet need due to historical lack of access, making risk scores based on historic utilization appear low. Combined with the cap on risk score growth in MSSP, these policies significantly underestimate the resources required to care for underserved beneficiaries and create financial challenges for ACOs providing this care.
Another challenge that ACOs frequently cite is the structure of the current Beneficiary Incentive Program (BIP), which lacks flexibility to tailor the program to the needs of an ACO’s population. While this program was established by Congress and will require statutory changes, there are opportunities for CMS to improve the process for updating waivers available in MSSP.
We urge CMS to avoid creating new requirements, which may limit ACOs’ flexibility to tailor to their unique populations and increase burden, and instead focus on addressing existing barriers. Rather than making changes to the patient-centeredness criteria, CMS could, for example, provide additional guidance and resources to ACOs looking to establish new partnerships with community stakeholders, and conduct outreach and provide support to CBOs interested in ACO partnerships. NAACOS looks forward to working with CMS and the ACO community to advance this important work.
Beneficiary Notification Requirements
While CMS does not propose any changes to the MSSP beneficiary notification requirements in this rule, NAACOS would like to reiterate concerns with the requirements as currently written and highlight key challenges ACOs face in implementing and complying with these requirements. Beneficiary notifications were required in the early years of MSSP, and the requirement was later removed due to the administrative burden, beneficiary confusion, and operational complexity caused by the notifications. CMS later reintroduced the requirement and made changes to the policies but has not addressed the fundamental issues with the requirement.
In last year’s rulemaking, CMS added a follow-up communication requirement in conjunction with the notice, which NAACOS opposed due to concerns it would exacerbate beneficiary confusion and operational complexity. ACOs have struggled in implementing this new element of the requirement and CMS did not provide any guidance on the follow-up requirement until April 2023, nearly four months after the requirement went into effect, and the guidance and FAQs provided failed to answer numerous questions about compliance or CMS’s expectations for ACOs. NAACOS has received dozens of questions and concerns about these requirements from ACO members, and from these we have outlined four overarching issues with the beneficiary notification requirements as currently written, detailed below.
First, ACOs that have elected preliminary prospective assignment with retrospective reconciliation (retrospective assignment) struggle to identify the denominator of beneficiaries to which they are required to provide the notice and follow-up. While ACOs with prospective assignment are only required to provide these to prospectively assigned beneficiaries, ACOs with retrospective assignment are required to provide them to all Medicare FFS beneficiaries. CMS provides these ACOs with information on preliminarily assigned (ALR Table 1-1) and assignable (ALR Table 1-6) beneficiaries but does not provide a list of or contact information for all FFS beneficiaries, making it infeasible for ACOs to identify and contact these beneficiaries to comply with the requirements. While CMS attempted to alleviate some burden by reducing the frequency with which ACOs must provide the notice, many ACOs’ compositions change significantly from year to year, with hundreds of new providers and thousands of new beneficiaries, making it incredibly challenging to identify all “new beneficiaries” each performance year. As such, some ACOs have expressed they may have to continue sending the notice to all beneficiaries in order to be compliant.
Second, the timing requirements of the initial notice and follow-up are impractical and make it effectively impossible to be fully in compliance. Under current regulations, ACOs are required to provide the notice at or before the first primary care service visit of the performance year and provide the follow-up “no later than the earlier of the beneficiary’s next primary care service visit or 180 days from the date the standardized written notice was provided.” Some beneficiaries will inevitably have a primary care visit on January 2 and ACOs do not receive attribution lists for the upcoming performance year until December, leaving very little time to send notifications by January 1. Requiring clinic staff to furnish the notice at point of care adds significant administrative burden—including staff training, changing workflows, and documenting and tracking when beneficiaries receive the notice—to primary care practices, many of which are experiencing staffing shortages and high levels of burnout.
The timing of the follow-up communication poses even more challenges. Many ACOs do not have access to practice-level scheduling data to determine whether the beneficiary’s next primary care visit takes place before the end of the 180-day period after the notice was provided. At a minimum, CMS should only require the follow-up communication within 180 days, removing “the next primary care service visit” as it is a difficult and impractical standard for all ACOs to track.
Third, lack of appropriate guidance from CMS and contradictory information provided by ACO coordinators have caused significant confusion among ACOs about how to comply with the requirements. As previously mentioned, written guidance documents from CMS fail to answer questions about implementation, required documentation, and what CMS considers to constitute compliance with the requirements. Additionally, because this guidance was not published until the second quarter of the year, some ACOs had to re-do many of the notifications to comply with the guidelines, adding costs and administrative burden. ACOs that have contacted their ACO coordinators with questions about these requirements have received information that contradicts answers provided by other ACO coordinators or conflicts with guidance and statements made by CMS.
For example, some ACOs were told by their ACO coordinators that the follow-up communication could be packaged with the initial notification (e.g., included as a cover letter or additional attachment with the standard written notice) while others were told it must be provided in a separate communication after providing the written notice. Later, CMS stated verbally that the follow-up communication must be provided on a separate day (calendar day vs. 24-hour period not specified) from the initial notice but has not included that information in any written guidance. Similarly, ACOs have received contradictory information on whether sending notices to potentially assignable (ALR Table 1-6) beneficiaries would satisfy the requirements. Given the broad confusion and contradictory information that has been provided to ACOs about these requirements, ACOs are concerned about compliance action in the event of an audit. ACO compliance officers dedicate time and resources to ensure ACOs are in compliance with MSSP regulations, and they cannot do this effectively if CMS cannot clearly define what is required of ACOs and what would satisfy an audit.
Finally, and perhaps most importantly, these requirements have caused confusion and frustration for Medicare beneficiaries, in direct contrast with the intention of the requirements. NAACOS strongly supports efforts to improve beneficiary education and engagement, and we are concerned to hear from ACOs, Medicare beneficiaries, and consumer advocates that the current beneficiary notifications are having the opposite effect.
As a result of the notifications, some beneficiaries choose to opt-out of data sharing without understanding what the data sharing process entails, making it difficult for ACOs to coordinate and manage patients’ care effectively. NAACOS members have reported that after sending the notice, many saw between 2 percent and 5 percent of patients opt-out of data sharing. The new follow-up communication has increased confusion and frustration. Some patients believe these communications are part of a scam, or that they have been enrolled in a managed care plan without their consent. ACOs have also reported that after providing the follow-up communication, they received a high volume of patient calls about clinical care, coverage issues, and questions about medication management, none of which were relevant to MSSP or appropriate for ACO operational staff to address.
Medicare beneficiaries and consumer advocates have also expressed concerns that these notifications do not resonate with patients and may exacerbate mistrust in the health care system. In a January 2023 panel discussion with Medicare ACO beneficiary board representatives, the representatives felt strongly that the current notice is not helpful and does not include information that matters to patients and expressed that CMS should take a more active role in educating beneficiaries about ACOs. One suggestion from the panel that NAACOS has also recommended is to provide information on ACOs and the benefits of the shift to value-based care in the “Medicare & You” handbook. The 2023 handbook contains no direct mention of MSSP and includes less than two pages on ACOs. In contrast, Medicare Advantage (MA) is mentioned twice in the table of contents alone and has an entire section of the handbook dedicated to detailing various plans and options available under MA and how to enroll. In order to engage beneficiaries in accountable care, the first step is to educate them about the existence of the program and what it means for their care. Not including comprehensive information in plain language about MSSP and ACOs broadly in the “Medicare & You” handbook is a missed opportunity to open the conversation about accountable care with beneficiaries.
NAACOS is a strong supporter of CMS’s goal to have all Medicare beneficiaries in a relationship with a provider accountable for their quality and total cost of care by 2030. Effectively communicating with and educating beneficiaries about accountable care will be essential to achieving this goal. NAACOS will continue to engage with CMS and other stakeholders, including patients and consumer advocates, to improve beneficiary communications as they are critical to expanding the reach of accountable care and to the success of patient engagement activities. We plan to convene a group of ACO leaders and consumer advocates to develop commonsense solutions to these challenges and we look forward to sharing the resulting recommendations with CMS.
Proposals to Align CEHRT Requirements for Shared Savings Program ACOs with MIPS
NAACOS strongly opposes CMS proposals to align CEHRT requirements for MSSP ACOs with MIPS and we urge CMS to reconsider this policy. By requiring all ACOs to report Promoting Interoperability, regardless of track or qualifying APM participant (QP) status, CMS is creating yet another disincentive for ACOs to participate in an Advanced APM and obtain QP status. CMS notes their intention with this proposal is to reduce burdens for ACOs, however the result is the opposite. Instead, CMS is now creating a new reporting obligation for ACOs who participate in an Advanced APM and obtain QP status. Lastly, QPs are statutorily excluded from the MIPS program and this proposal would essentially subject QPs to MIPS as Promoting Interoperability is the only reporting obligation ACOs have in the program.
Further, it would be difficult for ACOs to comply with this new requirement in the timeline proposed. The final rule will not be published until November, and ACOs must report to CMS those practices they wish to eliminate from their ACO participation list in September. This leaves ACOs no recourse if there are practices not currently on CEHRT that will be unable to comply with the new requirement by 2024. CMS must ensure ACOs still have the opportunity to bring small practices who are not currently on CEHRT into the ACO. ACOs can provide resources and assistance for transitioning to CEHRT, however this can take time, the current 75% attestation approach allowed ACOs to bring these practices into value arrangements We urge CMS to not finalize this proposal which would stifle growth in ACOs and take CMS further from their goal of having all patients in an accountable care relationship by 2030. Lastly, we urge CMS to provide additional information regarding the consequences of noncompliance with this requirement and how or whether the Promoting Interoperability score achieved will factor into compliance requirements.
QUALITY PAYMENT PROGRAM
Merit Based Incentive Payment System
MIPS Value Pathways (MVP) Reporting for Specialists in Shared Savings Program ACOs
NAACOS and its members have a shared interest in further engaging specialists in total cost of care models like ACOs. We do not feel this policy will bring CMS closer to its goals of furthering engagement of specialists in ACOs. We strongly oppose any requirement for specialists in an ACO to report MVP measures in addition to the quality measures the ACO is already reporting. Instead, to further support engagement of specialists in ACOs CMS must first address ACO needs to further this work by sharing data on cost and quality performance for specialists with ACOs and addressing policy and program design elements that currently are prohibitive to this work.
Request for Information on MIPS Incentives to Advance Alternative Payment Models
A key aim of the bipartisan Medicare Access and CHIP Reauthorization Act (MACRA) was to speed the transition to patient-centered, value-based care by encouraging physicians and other clinicians to transition into APMs. Today, approximately 30 percent of Medicare clinicians are participating in risk-based payment models, but the rate of uptake remains below original projections. While MACRA was a step in the right direction, more needs to be done to drive long-term system transformations. Stabilizing Medicare’s payment system and ensuring payment adequacy will also help physicians invest in the infrastructure and staffing necessary to transition into value-based models.
Overall, MACRA’s incentives have driven change in the Medicare payment system, but the incentive structure needs to be revisited for growth to continue. It’s clear that advanced APMs are transforming how patients in traditional Medicare receive care and achieving cost savings. If the 5 percent advanced APM incentive payments expire this year, and qualifying thresholds increase to unattainable levels, there will be a significant reduction in the move to value. Increasing thresholds and expiring incentives could result in a 32–42 percent drop in participation. A shift back to FFS for these clinicians could possibly increase total Medicare spending annually by $714 to 882 million. Additionally, successful transition to value-based care models requires clinicians to invest in workflow improvements, digital health tools, care coordinators, data analytics, quality measurement systems, transitional care services, and innovative patient engagement methods. While these advanced care delivery tools help improve patient care and outcomes, it is not without a cost. Incentive payments have been critical in helping clinicians make these initial investments and continue reinvesting in these care transformation initiatives that benefit patients.
CMS should work with Congress to provide an initial short-term extension of MACRA’s incentives and consider more sustainable longer-term incentive payments system that helps clinicians move away from standard FFS. Specifically, incentives are the building blocks to care transformation and CMS should consider the following:
- Decouple advanced APMs from the MIPS program and structure MIPS to incentivize participation in APMs.
- Redesign physician payment incentives to promote value by developing a three-tier system that provides increased flexibility and financial incentives for the adoption of value. The participation tracks should be:
- Fee-for-service (MIPS)—Clinicians that are not participating in any APM. MIPS should be revised so that the program does not incent remaining in FFS. Specifically, Congress should structure MIPS to have adequate payment adjustments for physicians but no additional incentives unless clinicians are taking steps to move to value.
- APMs—Clinicians participating in ACOs or other APMs that hold them accountable for cost and quality. Clinicians in this track should be exempt from MIPS quality reporting and only held to the quality and payment parameters of their model. Financial incentives should recognize the up front and ongoing investments needed to be successful in APMs.
- Advanced APMs—Clinicians participating in risk-based models. This track should have the strongest financial incentives and flexibility.
- New approaches should focus on simplifying the incentive structure, account for providers serving rural and underserved populations.
Within MIPS, CMS should use its current authority to further encourage the adoption of APMs by:
- Incorporating measures of population health readiness in MIPS. While the improvement activities contain some aspects of population health, it has not proved to be encourage APM adoption. CMS should examine how population health readiness can be infused across all categories.
- Provide additional technical assistance for providers who have not previously participated in APM arrangements.
- Reduce burden for ACOs who are included in MIPS. This includes not moving forward with the additional Promoting Interoperability requirement as proposed (detailed above), limiting annual changes to program criteria, focusing on more meaningful measurement, and providing more ACO-specific MIPS guidance.
Advanced Alternative Payment Models
QP Determinations
Until there is more universal participation in ACOs and APMs, NAACOS encourages the agency to finalize a policy where QP determinations can be made at both the APM entity and individual level. While the current QP thresholds can make it difficult for some ACOs to include specialists, we are concerned that only making QP determinations at the individual level could also discourage specialist participation in ACOs. Between 2020 and 2021 there was a modest 13 percent increase in the number of QPs qualifying for incentives and the average MSSP threshold score was roughly 46 percent for both payment and patient counts. As uptake of APMs continues to underperform original projections the agency should use a determination process that will maximize the number of QPs and promote growth in APMs.
Additionally, NAACOS is concerned that making QP determinations only at the individual level will increase burden as some clinicians in the ACO will qualify as QPs and others will not. This means the ACO will now have to support some clinicians with participation in MIPS. We recommend that the agency maintain the current attribution definition for determinations at the APM entity level and use the new proposed definition of attribution-eligible beneficiary for determinations at the NPI level. It is hard to determine the impact of the change for either APM entity or individual QP determination. We to ask CMS to produce some additional data on the impact of this definition change and specifically, the impact on ACOs.
Differential Conversion Factor Impact on Benchmarks
The current advanced APM incentive payments are not included in calculations for the purposes of rebasing ACO benchmarks nor are they counted as expenditures for the ACO. NAACOS is concerned that under current law when QPs receive the higher 0.75 percent conversion factor update beginning in payment year 2026, it will become more difficult for ACOs to reduce spending below benchmarks. This is because ACO benchmarks are based on national and regional spending trends. Since most providers are still participating in MIPS, benchmarks will be reflective of the lower 0.25 payment updates. NAACOS encourages the agency to evaluate the potential impact the differential conversion factor may have on ACOs ability to meet benchmarks. We also encourage the agency to issue a request for information in the next fee schedule to seek stakeholder input to help the agency develop proper safeguards. With participation in APMs already lagging original projections, it’s important to ensure that payment updates for clinicians do not negatively impact their financial performance in their models.
CONCLUSION
Thank you for the opportunity to provide feedback on CY2024 Physician Fee Schedule and MSSP proposed rule. NAACOS and its members are committed to providing the highest quality care for patients while advancing population health goals for the communities they serve. We look forward to our continued engagement on improving and enhancing MSSP. If you have any questions, please contact Aisha Pittman, senior vice president, government affairs at [email protected].
Sincerely,

Clif Gaus, Sc.D.
President and CEO
NAACOS
