NAACOS Newsletter for Members and Partners March 25, 2021
| MACRA ALERT: WILL YOUR ACO QUALIFY FOR THE 5% AAPM BONUS IN 2022? Nearly 40 percent of ACOs will participate in a qualifying Advanced Alternative Payment Model (Advanced APM) in 2022—allowing their physicians and other clinicians to be eligible to earn a 5 percent bonus if the ACO meets Qualifying APM Participant (QP) thresholds. NAACOS successfully lobbied Congress to freeze the QP thresholds at 35 percent (patient count) and 50 percent (payment) for Performance Years (PY) 2021 and 2022. But, one in five of Advanced APM ACOs could still fail to meet the QP thresholds. If your ACO is in an Advanced APM track or thinking of joining one in 2022, the Institute for Accountable Care can help you plan by estimating your ACO’s 2022 QP score—and importantly—providing estimates for each of your ACO’s physician groups/participant TINs. We can also model the impact of adding or removing specific physician groups/participant TINs on your ACO’s QP score. These services are provided for a fee. Get more information or contact us. NAACOS SURVEY REVEALS CONCERNS ABOUT MSSP QUALITY OVERHAUL NAACOS recently surveyed Medicare Shared Savings Program (MSSP) ACOs to collect feedback on the MSSP quality overhaul and to understand ACO readiness to shift from the Web Interface reporting option to electronic clinical quality measures (eCQMs) and MIPS Clinical Quality Measures (CQMs). The quality overhaul was finalized in the final 2021 Medicare Physician Fee Schedule Rule, with some changes effective in 2021 and others being implemented starting in 2022. NAACOS has been actively engaged with CMS seeking to change a number of aspects of the quality overhaul and the survey findings will be very helpful in our advocacy. There were 200 responses from 163 ACOs across the country, representing a quarter of MSSP ACOs. As shown in the graph below, almost 75 percent of ACOs are either “extremely concerned” or “very concerned” about the requirements to implement eCQMs and MIPS CQMs in 2022. 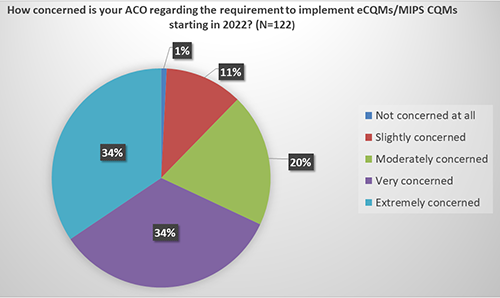 Other findings included:
QUALITY IS KEY AT THE NAACOS SPRING 2021 CONFERENCE! Join us for the NAACOS 2021 Spring Conference April 20–30. Hear from CMS on Tuesday, April 27, in the Review of MSSP ACO Quality Overhaul session where CMS speakers will walk through these changes, answer ACO questions and provide clarification on key quality concepts affecting ACOs. The session will also include ACO speakers sharing their strategies for meeting the new requirements. Congratulate the winners of the 2021 NAACOS Leaders in Quality Excellence Award and hear from the three organizations about their exemplary efforts in quality improvement and disseminating best practices. This session will take place Thursday, April 22, from 3:00–4:00 pm ET, where you will hear from each of these organizations:
Don’t Miss the Opportunity to Network with ACOs! The Spring 2021 Virtual Conference will feature a virtual exhibit hall where attendees will be able to meet with exhibitors online! Features will include virtual meet-ups, virtual networking, product photos, and MUCH more! Opportunities for vendors include sponsorship packages designed to maximize this virtual format. NAACOS Partners are the only non-ACOs allowed to exhibit and sponsor NAACOS conferences. Reserve your space today! |
|
|
|
NAACOS WRITES NEWLY CONFIRMED HHS SECRETARY XAVIER BECERRA In a letter congratulating newly confirmed HHS Secretary Xavier Becerra, NAACOS urged HHS to continue to transition our health system to reward value. This could be achieved by:
SEEKING ACOS INTERESTED IN A PHYSICIAN VALUE CHAMPION TRAINING CURRICULUM The Institute for Accountable Care, NAACOS research and data arm, is looking for ACOs interested in an evidence-based physician leadership training program designed to promote high-value care and reduce the use of low-value care. This project will focus specifically on patients with dementia, although the skills are transferable to other population groups or areas of low value care. Participants for this project will join in 10 one-hour training webinars led by Dr. Michael Parchman from Kaiser Permanente and also participate in an National Institute on Aging evaluation (if funded). We are specifically seeking ACOs with multiple primary care practice sites willing to participate in a rigorous study. For more information, please contact Jennifer Perloff from the Institute for Accountable Care. CMS CLARIFIES ACOS’ COVID-19 PHE PROTECTIONS EXTEND INTO 202 CMS recently updated FAQs on COVID-19, clarifying shared losses for MSSP ACOs will be reduced based on the proportion of months in 2021 that are covered by the public health emergency (PHE). NAACOS had sought this clarity since CMS rulemaking last year didn’t clearly state what ACO-specific adjustments would be made if the ongoing COVID-19 PHE extended into 2021. CMS’s clarification includes ACOs unable to report quality, stating they will have their quality score set equal to the 30th percentile MIPS Quality performance category score. CMS is still evaluating the impact the COVID-19 PHE had on MSSP ACOs’ quality reporting for 2019 in order to determine an approach for the Quality Measures Validation audit. More NAACOS information on COVID-19 and ACOs is available.  CONGRESS TURNS TO NEXT ROUND OF POLICIES Following the passage of the American Rescue Plan earlier this month, Congress has turned to its next agenda items for the 117th Congress. On the docket will be a reported $3 trillion plan for new spending, including infrastructure projects, regulations to reduce carbon omissions, and social economic policies. It is anticipated that drug pricing measures and tax increases are under consideration to finance the plan, which may be divided into separate measures for congressional consideration. Also this week, congressional committees are continuing their examination of Affordable Care Act expansion and COVID response, and the Senate is expected to take up a House-passed bill (H.R. 1868) waiving statutory requirements to offset the nearly $1.9 trillion American Rescue Plan and extend the March 31 suspension of Medicare sequestration cuts until the end of the year. Lastly, since HHS Secretary Becerra was confirmed by the Senate last week, additional HHS appointees are expected to move through the confirmation process in the April work period, including Andrea Palm, nominee for HHS Deputy Secretary, and Chiquita Brooks-LaSure, nominee for CMS Administrator. NAACOS TO HOST TWO DIRECT CONTRACTING EDUCATIONAL WEBINARS It’s not too late to register for this week’s Direct Contracting Learning Discussion. This collaborative discussion will provide a forum for shared learning, so please bring questions, feedback, and stories. NAACOS is hosting this forum to help members who are gearing up for Direct Contracting participation starting in April as well as those weighing their participation options for 2022. Registration is free for NAACOS members. NAACOS will also host a webinar on April 6 to review the basic structure of the Direct Contracting Model, including key updates over the Next Generation ACO Model and differences with MSSP. Attendees can also expect to learn about the model’s financial methodology, capitation options and benefit enhancements. While NAACOS has held similar model overview webinars in the past, this one includes new details recently released by CMS such as those from the Performance Agreements for 2021. This “101” webinar will serve as a primer for more in-depth discussions set to take place during our spring conference in April. Registration is free for NAACOS members. MSSP QUALITY REPORTING DEADLINE LOOMS The MSSP quality reporting submission deadline is Wednesday, March 31, 2021. CMS will automatically accept the data entered in the Quality Payment Program (QPP) site as of Tuesday, March 31, 2020, at 8:00 pm ET. This information will be considered an ACO’s final submission. As a reminder, ACOs must have an appropriate user role associated with their organization with a Health Care Quality Information System (HCQIS) Access Roles and Profile (HARP) User ID and password to complete the submission process. Additionally, for ACOs subject to the Merit-based Incentive Payment System (MIPS), the deadline for clinician practices and individual eligible clinicians (ECs) to submit their Promoting Interoperability (PI) data is also Wednesday, March 31, 2021. Practices and clinicians will report and attest to PI data also via the QPP site. Hospitals and Medicaid Eligible Professionals (EPs) also report PI data under separate hospital PI rules and requirements; the acute hospital, critical access hospital and Medicaid PI reporting deadline to submit is Thursday, April 1, 2021. More information on the hospital and Medicaid PI requirements are available. |
|
|
|
NAACOS RESOURCE HIGHLIGHTS ACO SAVINGS IN 2019 NAACOS recently released a new resource that highlights MSSP and Next Generation ACO savings in 2019, as well as Medicare ACOs’ historical contributions. Since 2012, ACOs have saved Medicare $8.5 billion and $2.5 billion after accounting for shared savings payments, shared loss payments, and discounts to CMS. Data show these ACOs continued to provide high-quality care and yield satisfied patients. This document illustrates the meaningful work of ACOs. NAACOS hopes to use this document to highlight the success of the ACO model and to urge policymakers to enact policies to support ACOs. PRIMARY CARE FIRST ROUND TWO RFA AVAILABLE CMS recently released the Request for Applications (RFA) for the second cohort of the Primary Care First (PCF) Model. The RFA is available and more information, including upcoming webinars on Cohort 2 are available. PCF Cohort 2 will have five performance years and is scheduled to begin in January 2022. Earlier this year, CMS announced a number of eligibility changes for the second PCF cohort, notably that practices in the 26 eligible PCF regions may apply regardless of participation in the Comprehensive Primary Care Plus (CPC+) Model, which was initially a requirement. The agency also recently announced it is reviewing the Seriously Ill Population component of the model and that will not begin in April, as was previously planned. Consistent with Tracks 1 and 2 of the CPC+ Model, practices participating in ACOs under all MSSP tracks are eligible to participate in PCF. In contrast, providers participating in the Direct Contracting Model may not simultaneously participate in PCF. MEDPAC PUBLISHES ITS MARCH REPORT TO CONGRESS The Medicare Payment Advisory Commission (MedPAC) recently released its March report to Congress, and there are a couple of chapters relevant to ACOs and value-based care. The commission recommends policymakers continue covering telehealth services as it has during the COVID-19 PHE for one-to-two years after the PHE ends to gather more information on telehealth quality and costs. That additional information will inform any permanent changes that need to be made. In the chapter, MedPAC spells out how Advanced APMs could be an avenue to wider telehealth coverage but notes there are administrative complexities, including around knowing which patients are assigned to ACOs—and therefore eligible for telehealth visits—and which are not. NAACOS supports allowing greater flexibility in telehealth use for all ACOs, regardless of risk level or choice of attribution. MedPAC also estimates that Medicare payments to Medicare Advantage plans will be 104 percent of fee-for-service spending in 2021 because of intensive coding practices. The commission has tried to draw attention to the fact that Medicare Advantage has never saved the federal government money, despite ongoing debate around rising federal health spending. The full MedPAC report and press release are available online. INNOVATION CENTER ANNOUNCES ET3 PARTICIPANTS The Center for Medicare and Medicaid Innovation (Innovation Center) recently announced the final list of participants for the Emergency Triage, Treat, and Transport (ET3) Model, which tests paying ambulance services for treating patients at a scene, transporting to non-emergency department, or treating via telemedicine. The list includes 184 public and private ambulance providers and suppliers representing 36 states. CMS also issued a Notice of Funding Opportunity (NOFO) of up to $34 million over two years for local and state governments to expand emergency and non-emergency medical triage services in locations of model participants. Those applications are due May 11 at 3:00 pm ET. While only ambulance services are eligible to participate, ACOs could coordinate with ambulance providers in their markets on how to best direct ACO patients to the most clinically appropriate, high-quality, and cost-effective setting. |
