Statement for the Record
Senate Finance Committee
Hearing to Consider the Nominations of Andrea Joan Palm to be Deputy Secretary of Health and Human Services and Chiquita Brooks-LaSure to be Administrator of the Centers for Medicare & Medicaid Services
April 15, 2021
The National Association of ACOs (NAACOS) appreciates the opportunity to express our views on the nomination of Andrea Joan Palm to be Deputy Secretary of the Department of Health and Human Services (HHS) and Chiquita Brooks-LaSure to be Administrator of the Centers for Medicare & Medicaid Services (CMS). We strongly support the nominations of Ms. Palm and Ms. Brooks-LaSure and are hopeful that they and the Committee will consider the following issues in their work ahead.
NAACOS represents more than 12 million beneficiary lives through hundreds of organizations participating in population health-focused payment and delivery models in Medicare, Medicaid, and commercial insurance. Models include the Medicare Shared Savings Program (MSSP), the Next Generation Model, the Direct Contracting Model, and alternative payment models supported by a myriad of commercial health plans and Medicare Advantage. NAACOS is a member-led and member-owned nonprofit organization that works to improve quality of care, outcomes, and healthcare cost efficiency.
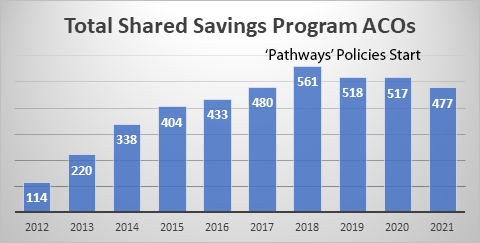
NAACOS looks forward to working collaboratively with the Committee and today’s nominees on these topics. Mostly notably, we hope these appointments will bolster the shift to value following recent years of policies that have hampered that critical transition. The transition to value should not be taken for granted. While much progress has been made in the past decade, this transformation is threatened. For example, according to new data released by CMS, the number of participants in the largest and most successful value-based payment model, the MSSP, reached its lowest level since the Trump administration took office four years ago. As shown below, to start 2021, 477 ACOs are participating in the MSSP, down from a high of 561 in 2018 and the lowest since 480 participated in 2017, the Trump administration’s first year in office.
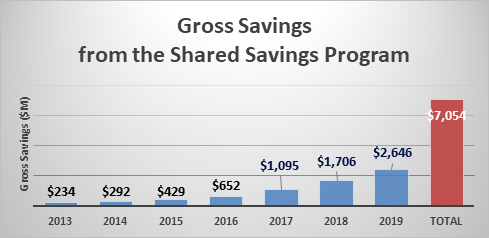
In contrast to the diminishing number of ACOs, the MSSP continued to produce greater savings every year and saw its best year yet in 2019, the most recent year for which data is available. Serving 11.2 million seniors in 2019, the MSSP saved Medicare $2.6 billion and $1.2 billion after accounting for shared savings bonuses and collecting shared loss payments. Gross savings are shown below.
The Next Generation ACO Model, the premier accountable care model ran out of the CMS Innovation Center that emphasizes high risk and high reward, has also demonstrated great results. Serving 1.2 million patients in 2019, the model saved $559 million compared to the CMS-generated benchmarks and netted $204 million to the Medicare Trust Fund after accounting for shared savings, shared losses, and discounts paid to CMS. NAACOS urges CMS to extend the Next Gen model through 2022, giving time to install it as a permanent option for ACOs, either as a stand-alone track or option within MSSP. The model is scheduled to sunset at the end of 2021. The above results should speak for themselves and substantiate permanentizing.
Given the success of the ACO program and need to strongly support the transition to value-based care and payment, we request HHS re-examine the balance of risk and reward for ACOs to bolster ACO growth and therefore savings to Medicare and to support high quality, coordinated patient care. Among those changes, we request that HHS and CMS reverse certain policies from a 2018 MSSP overhaul, which CMS called the ACO “Pathways to Success.” That overhaul included some damaging provisions such as a cut to the share of savings most ACOs are eligible to keep and a push for ACOs to assume risk too quickly. These policies have chilled ACO growth and should be changed.
NAACOS also recommends that HHS focus the value transition on providers, keeping them at the center of payment models instead of implementing programs and policies to attract new players into traditional Medicare. As a telling example of CMS’s recent approach, in 2018 the agency released a model initially titled “Direct Provider Contracting,” only to later drop the word “Provider.” That name change went along with an emphasis on giving favorable treatment to entice new participants, such as payers, to the model at the expense of those who have been on the frontlines of the value transition for the past decade.
To support the ACO movement and recalibrate the value transition to center on and support healthcare providers, NAACOS recommends the following:
To make progress on the broader goals listed above, NAACOS recommends enacting the following specific policy change this year:
Ultimately, President Biden’s administration inherits fewer ACOs than the Obama administration left at the start of 2017, which is a trend NAACOS hopes will be reversed under your leadership at HHS. We appreciate the work of the Committee on these topics and look forward to working with the nominees.
